Connect With Us
Super User
Surgery for Diabetic Peripheral Neuropathy

Diabetic peripheral neuropathy, or DPN, is a common complication of diabetes. It occurs when high blood sugar levels damage the nerves, especially those in the legs and feet. DPN can lead to various symptoms, including numbness, tingling, burning sensations, and pain in the affected areas. It can also cause muscle weakness and affect balance and coordination. Over time, it can have serious complications if not managed properly. Surgery to release nerves in the legs has been shown to help people with this affliction and researchers have found that when people had such surgery, they experienced less pain and had an improved ability to feel touch. Surgery on a specific nerve in the tarsal tunnel area seemed to work best in these cases, and those who underwent such surgery were less likely to get ulcers or need amputation. If you suffer from DPN, it is strongly suggested that you make an appointment with a podiatrist for a full evaluation and treatment. Surgery may or may not be right for you, but new developments are constantly being made in this area that can potentially be helpful.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact one of our podiatrists of Podiatry Care Specialists. Our doctors will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Surgery
In most cases, foot surgery is often chosen as the last available option for conditions that have otherwise been unsuccessfully treated. Surgery may be necessary for several reasons, including the removal of foot deformities (e.g. bone spurs or bunions), arthritis problems, reconstruction due to injury, and congenital malformations (e.g. club foot or flat feet). Regardless of one’s age, foot surgery may be the only successful option for treatment for certain conditions.
The type of surgery one undergoes depends on the type of foot condition the patient has. For the removal of a bunion growth, a bunionectomy is necessary. If the bones in the feet need to be realigned or fused together, a surgical fusion of the foot is needed. For pain or nerve issues, a patient may require surgery in which the tissues surrounding the painful nerve are removed. Initially, less invasive treatments are generally attempted; surgery is often the last measure taken if other treatments are unsuccessful.
While in many cases surgery is often deemed as the final resort, choosing surgery comes with certain benefits. The associated pain experienced in relation to the particular condition is often relieved with surgery, allowing patients to quickly resume daily activities. The greatest benefit, however, is that surgery generally eliminates the problem immediately.
Podiatry history has shown that foot treatments continue to evolve over time. In the field of foot surgery, endoscopic surgery is just one of the many advanced forms of surgery. As technology vastly improves so too will the various techniques in foot surgery, which already require smaller and smaller incisions with the use of better and more efficient tools. Thanks to such innovations, surgery is no longer as invasive as it was in the past, allowing for faster and easier recoveries.
Risk Factors of Gout in Women

Gout, a type of arthritis characterized by sudden, severe joint pain and inflammation, has often been associated with men. However, it is important to recognize that women are not immune to this painful condition. While women have a lower overall risk of developing gout compared with men, certain factors can increase their susceptibility. One significant risk factor is age. Women are more likely to develop gout after menopause when estrogen levels drop. Hormonal changes can affect uric acid levels, contributing to the formation of gouty crystals in the joints. Additionally, obesity is a prominent risk factor for both genders. Women with a higher body mass index are more likely to develop gout, as excess weight can lead to elevated uric acid levels. Certain medications, such as diuretics or low-dose aspirin, can also raise the risk of gout in women. Genetics and a family history of gout may contribute to the development of this condition. If a woman has relatives with gout, her chances of developing the condition are higher. Maintaining a healthy lifestyle, managing weight, staying hydrated, and addressing underlying medical conditions can help reduce the risk of gout in women. If you would like more information about women developing gout, it is suggested that you consult a podiatrist who can provide you with the knowledge you are seeking.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact one of our podiatrists from Podiatry Care Specialists. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes of Running Injuries

Running is thought to be a good way to stay fit and healthy, but it also comes with risks. Foot and ankle injuries are all too common among runners. Overuse is a prevalent issue, usually stemming from pushing your body too hard or increasing your mileage too quickly. These actions can lead to problems like plantar fasciitis, Achilles tendonitis, and stress fractures. Poor footwear choices also play a significant role in causing foot or ankle injuries. Worn-out or ill-fitting shoes fail to provide the necessary support and cushioning, increasing the risk of injuries. Ensuring your shoes are the right fit for your feet and running style is important. Inadequate warm-up routines can strain the muscles and ligaments, making them more susceptible to injuries. In addition, running on uneven terrain can increase the likelihood of twisting an ankle. Biomechanical issues, such as overpronation or supination, can place extra stress on your feet and ankles, making them prone to injury. If you experience persistent pain or discomfort as a result of your running activity, it is suggested that you consult a podiatrist for an exam, diagnosis, and treatment options.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact one of our podiatrists of Podiatry Care Specialists. Our doctors will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Reasons to See a Podiatrist

Foot and ankle issues, from various causes like chronic conditions or ill-fitting shoes, can interfere with daily life. Consulting a podiatrist is important for conditions like joint pain, often accompanied by swelling, redness, stiffness, or tenderness, which could be due to arthritis. Diabetes increases the risk of foot problems, from dry skin to severe complications like neuropathy, and regular podiatrist foot exams significantly lower amputation risks. Persistent heel pain caused by things like heel spurs or inflamed tendons requires a podiatrist's diagnosis and tailored treatment. Stubborn ingrown toenails, a common issue, may lead to infection and a podiatrist can provide timely treatment, including nail removal in chronic cases. Suspected foot or ankle injuries, such as sprains or strains, demand prompt diagnosis and treatment. Corns and calluses, if left untreated, can be painful and a podiatrist can safely remove them and offer prevention advice. Runners prone to issues like shin splints benefit from a podiatrist's assessment and recommendations for suitable athletic footwear. Painful bunions worsen without treatment, and a podiatrist can suggest measures like padding, taping, or orthotics. Suspected athlete's foot, a fungal infection causing itchiness and scaliness between the toes, requires professional care if over-the-counter treatments do not work. If you have any sort of foot or ankle problems, it is suggested that you make an appointment with a podiatrist who can address these concerns, and offer diagnosis, treatment, and preventative guidance to enhance mobility and well-being.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact one of our podiatrists from Podiatry Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
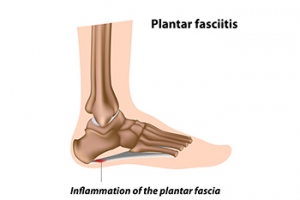
Causes, Symptoms, and Possible Relief Options for Plantar Fasciitis

Plantar fasciitis, a common and often distressing foot condition, can disrupt daily routines with its sharp heel pain. This ailment arises from inflammation of the plantar fascia, which is the tissue connecting the heel bone to the toes. Causes can vary, including repetitive stress, wearing poor-fitting footwear, and obesity. Symptoms can manifest as intense pain upon waking or after periods of rest, and gradually easing with movement. Relief techniques can include performing stretching exercises targeting the calf muscles and plantar fascia, helping to relieve tension. Orthotic shoe inserts can provide support and distribute pressure. Taking anti-inflammatory medications can be beneficial, and for more severe cases, medical interventions such as surgery may be considered. By addressing the underlying triggers and adopting a combination of remedies, individuals can gradually step back into pain-free mobility. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can effectively treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Podiatry Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Unmasking the Causes of Athlete’s Foot

Athlete's foot, medically known as tinea pedis, is a common fungal infection that primarily affects the feet. This condition is caused by various dermatophyte fungi that thrive in warm, damp environments like communal showers, swimming pools, and locker rooms. The fungus can also spread through contact with infected individuals or contaminated surfaces. Certain factors increase the risk of developing athlete's foot. Athletes, hence the name, are particularly vulnerable due to the frequent use of communal spaces. In addition, individuals who wear tight-fitting shoes or synthetic socks that trap moisture are at higher risk. Maintaining proper foot hygiene, wearing breathable footwear, and avoiding prolonged exposure to damp conditions are essential preventive measures. If you have developed athlete’s foot, it is suggested that you consult a podiatrist who can guide you toward effective treatment measures.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our podiatrists from Podiatry Care Specialists. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.