Connect With Us
Super User
Heel Pain Caused by Plantar Fasciitis
Plantar fasciitis, the most common type of heel pain, is typically caused by overuse of the plantar fascia—the fibrous tissue on the sole of the foot that connects the heel bone with the toes. This condition occurs when the plantar fascia gets overly stretched or damaged, including small tears where this connective tissue joins with the heel bone. Plantar fasciitis causes stabbing pain on the bottom of the heel. It is often worse in the morning when you first wake up, since the plantar fascia has tightened overnight. As you begin stretching the plantar fascia with regular movement, the pain usually lessens, only to increase again as the day progresses. Plantar fasciitis can happen to anyone who overloads the plantar fascia through excessive exercise, obesity or pregnancy and wearing improper footwear, as well as those with diabetes or structural abnormalities in the feet. Podiatrists have many effective treatments for plantar fasciitis. If you are experiencing heel pain, it's a good idea to make an appointment with a podiatrist near you.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Podiatry Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Choosing Work Footwear That Works
Here are a few tips on finding the perfect fit in your work boots or work shoes. First, the shoe/boot should be snug, but not tight. The back of the shoe or boot should hug (but not cut into) the heel, and the ball of your foot should lay comfortably in the ball of the shoe. There should be space between the tips of the toes and the toe box. Your toes should have enough room to move a bit and they should never be squeezed or confined. Work shoes and boots that fit properly will keep you energized and even help your footwear last. For more tips on work footwear or to learn about custom orthotics that can keep your feet comfortable and healthy, contact your local podiatrist.
It is important to find shoes that fit you properly in order to avoid a variety of different foot problems. For more information about treatment, contact one of our podiatrists from Podiatry Care Specialists. Our doctors will treat your foot and ankle needs.
Proper Shoe Fitting
Shoes have many different functions. They cushion our body weight, protect our feet, and allow us to safely play sports. You should always make sure that the shoes you wear fit you properly in order to avoid injuries and deformities such as: bunions, corns, calluses, hammertoes, plantar fasciitis, stress fractures, and more. It is important to note that although a certain pair of shoes might be a great fit for someone else, that doesn’t mean they will be a great fit for you. This is why you should always try on shoes before buying them to make sure they are worth the investment. Typically, shoes need to be replaced ever six months to one year of regular use.
Tips for Proper Shoe Fitting
- Select a shoe that is shaped like your foot
- Don’t buy shoes that fit too tight, expecting them to stretch to fit
- Make sure there is enough space (3/8” to ½”) for your longest toe at the end of each shoe when you are standing up
- Walk in the shoes to make sure they fit and feel right
- Don’t select shoes by the size marked inside the shoe, but by how the shoe fits your foot
The shoes you buy should always feel as good as they look. Shoes that fit properly will last longer, feel better, and improve your way of life each day.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Get a Proper Shoe Fit
Many people suffer from foot problems because their shoes are poorly fitted. When shopping for a new pair of shoes, fashion usually triumphs over comfortability. A pair of well fitted shoes is essential in preventing foot problems and potential injuries.
Poorly fitted shoes can cause foot issues such as plantar fasciitis, bunions, hammertoes, ingrown toenails, and foot pain. Shoes such as high heels and sandals may cause problems for your feet. These shoes put the foot in an unnatural position for long periods and fail to provide good foot support. It is recommended to not wear either one for an extended period.
When you are trying on shoes, make sure they have enough space for your toes to move around. Shoes shouldn’t be cramped but also shouldn’t have too much room that your foot moves around in them. A snug shoe is a good choice. They should also provide good arch support and cushioning. Athletic shoes tend to offer both good support and cushioning. A degree of flexibility is necessary so they aren’t too stiff or too unsupportive.
If you can wear your shoes for a long period of time without experiencing any discomfort, this is a sign that your shoes fit properly. Do not be too dismayed if the shoe isn’t a perfect fit at first; many shoes take a few days to weeks to properly break in. However don’t expect an uncomfortable shoe to become fitted to your foot.
For those with foot conditions such as flat feet or pronation, orthotics may be helpful or even necessary to prevent foot pain. Orthotics are inserts that are placed in the shoe and provide support and cushioning for the foot. While there are many types of orthotics out there, custom-made orthotics may be necessary depending upon your foot and foot conditions.
Feet change in size over time. It is important to check your foot size over time so that you can make sure you have the perfect fit for your feet. A podiatrist can provide more information on proper shoe fitting and foot orthotics.
Pins and Needles in Your Feet
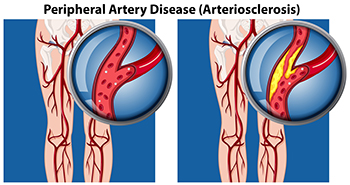
Many people experience the sensation of “pins and needles” in their feet when they cross their legs for too long. Generally, it recedes once the blood flows to the affected area. However, when the occurrence of this sensation becomes more frequent, it can affect your ability to walk or stand safely. This condition, known as paresthesia, may be experienced as tingling, itching and burning, aching pain, or numbness. The cause is likely to be peripheral artery disease (PAD), which is a buildup of plaque in your arteries. The result is poor circulation due to the reduced flow of blood to the feet. Other contributing factors include having diabetes, being overweight, overindulgence in alcohol, and possible vitamin deficiency. Some actions that might help are eating healthy foods, avoiding alcoholic beverages, and taking short walks daily. If you have noticed an increase in the frequency of a pins-and-needles sensation in your feet, it is a good idea to make an appointment with a podiatrist as soon as possible for a complete examination and suggested treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Podiatry Care Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Why Does My Ankle Feel Unstable?
 Many athletes, and others, who have previously sprained an ankle, may frequently experience their ankle giving way on the outer side. This may be a case of chronic ankle instability. The condition normally occurs when doing an activity, but in some cases it can happen even while you are standing still. Symptoms include turning the ankle during sports or other activities, swelling, pain, and a wobbly feeling in the ankle. This instability may be caused by stretched ligaments from a sprain that has not fully healed. Treatment can involve exercises to strengthen the muscles around the affected area, wearing a brace to increase joint support, and taking certain medications. It would be wise to consult a podiatrist if you are experiencing ankle instability to determine the extent of treatment that is necessary. In some cases, surgery may be an alternative, and after an exam your podiatrist can review the options.
Many athletes, and others, who have previously sprained an ankle, may frequently experience their ankle giving way on the outer side. This may be a case of chronic ankle instability. The condition normally occurs when doing an activity, but in some cases it can happen even while you are standing still. Symptoms include turning the ankle during sports or other activities, swelling, pain, and a wobbly feeling in the ankle. This instability may be caused by stretched ligaments from a sprain that has not fully healed. Treatment can involve exercises to strengthen the muscles around the affected area, wearing a brace to increase joint support, and taking certain medications. It would be wise to consult a podiatrist if you are experiencing ankle instability to determine the extent of treatment that is necessary. In some cases, surgery may be an alternative, and after an exam your podiatrist can review the options.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with one of our podiatrists from Podiatry Care Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ways to Treat Toenail Fungus
 Signs that you may have contracted a fungal toenail infection are rather easy to spot. Typically, you will notice a whitening or yellowing of the nail, and it will appear to be thicker and more brittle. The fungus, known as onychomycosis, is often spread in swimming pools, saunas, gyms, or nail salons – places where you are likely to walk barefoot. Tight socks that hold in moisture may also be a contributing factor. Heat, humidity, and perspiration help spread the infection, which is highly contagious. A few natural remedies that may help reduce the fungus from spreading include applying tea tree, lavender, lemon, or thyme oils to the affected nails. A foot bath with baking soda or white vinegar may help too. However, if the nail condition persists or spreads it is suggested that you consult with a podiatrist for an examination and treatment plan.
Signs that you may have contracted a fungal toenail infection are rather easy to spot. Typically, you will notice a whitening or yellowing of the nail, and it will appear to be thicker and more brittle. The fungus, known as onychomycosis, is often spread in swimming pools, saunas, gyms, or nail salons – places where you are likely to walk barefoot. Tight socks that hold in moisture may also be a contributing factor. Heat, humidity, and perspiration help spread the infection, which is highly contagious. A few natural remedies that may help reduce the fungus from spreading include applying tea tree, lavender, lemon, or thyme oils to the affected nails. A foot bath with baking soda or white vinegar may help too. However, if the nail condition persists or spreads it is suggested that you consult with a podiatrist for an examination and treatment plan.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our podiatrists of Podiatry Care Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
What Do Podiatrists Do?
Podiatrists are physicians, and often surgeons, who have studied the foot, ankle, and lower leg, along with all associated ailments. They have received an undergraduate degree as well as medical degree and undergo four years of postgraduate study with a three-year residency. They treat a variety of foot and ankle issues, including fungal and ingrown toenails, heel pain, fractures, ankle sprains and strains, nerve damage (neuromas), bunions, hammertoe, arthritis, wound care, and complications of the feet due to diabetes and peripheral artery disease, and much more. They can also perform surgeries to treat certain foot and ankle conditions, perform gait analyses, and fit and create custom orthotics for their patients. If you experience any discomfort in your feet or ankles or are having a hard time getting around, make an appointment with a podiatrist who can get to the bottom of your condition and treat it accordingly.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Podiatry Care Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in West Chester, and Broomall, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.